Quality Measures
Supported Measures
Measure Set Selectors
-
All
Measures
-
Ambulatory (EC/EP)
- eCQMs
- MIPS
-
MVP
- Advancing Cancer Care (M0001)
- Mental Health & Substance Use (M1369)
- Rehabilitative Support for Musculoskeletal Care (M1370)
- CCBHC
- UDS
-
Inpatient
- Inpatient Quality Reporting (IQR)
- The Joint Commission
- Outpatient
-
Ambulatory (EC/EP)
DHIT’s Quality Measure Capabilities

Calculate and display measure performance
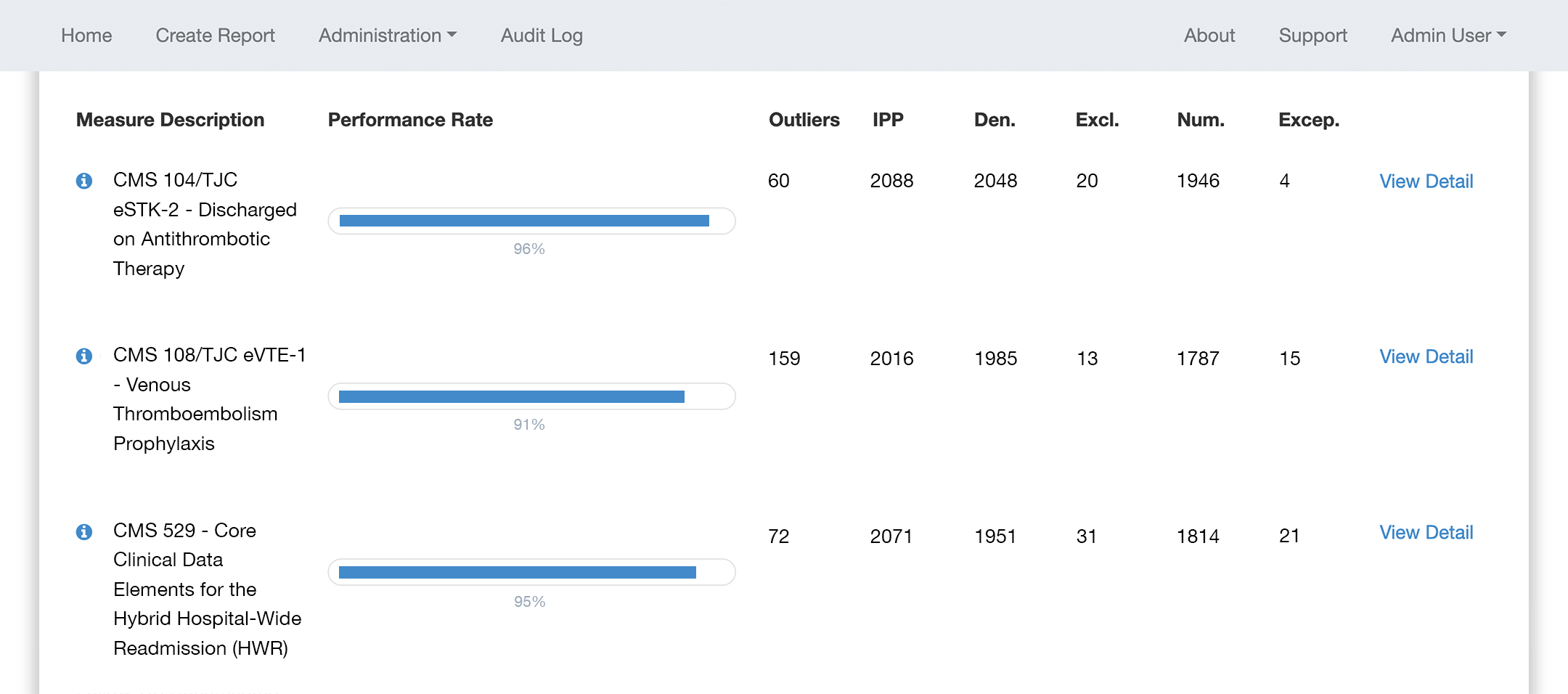
Output results to QRDA (XML) or JSON, or use DHIT to easily submit to QPP, IQR, or The Joint Commission
Software
Whether you’re reporting CQMs to CMS, The Joint Commission, or both, we can guide you through the testing, file validation and submission process. We provide full services for ONC Certification, MIPS, Hospital Quality Reporting and ORYX (The Joint Commission).
CQMsolution
DHIT’s CQMsolution software supports all eCQMs. Optimize your measure performance by calculating, displaying, and analyzing Quality Measures with ease.

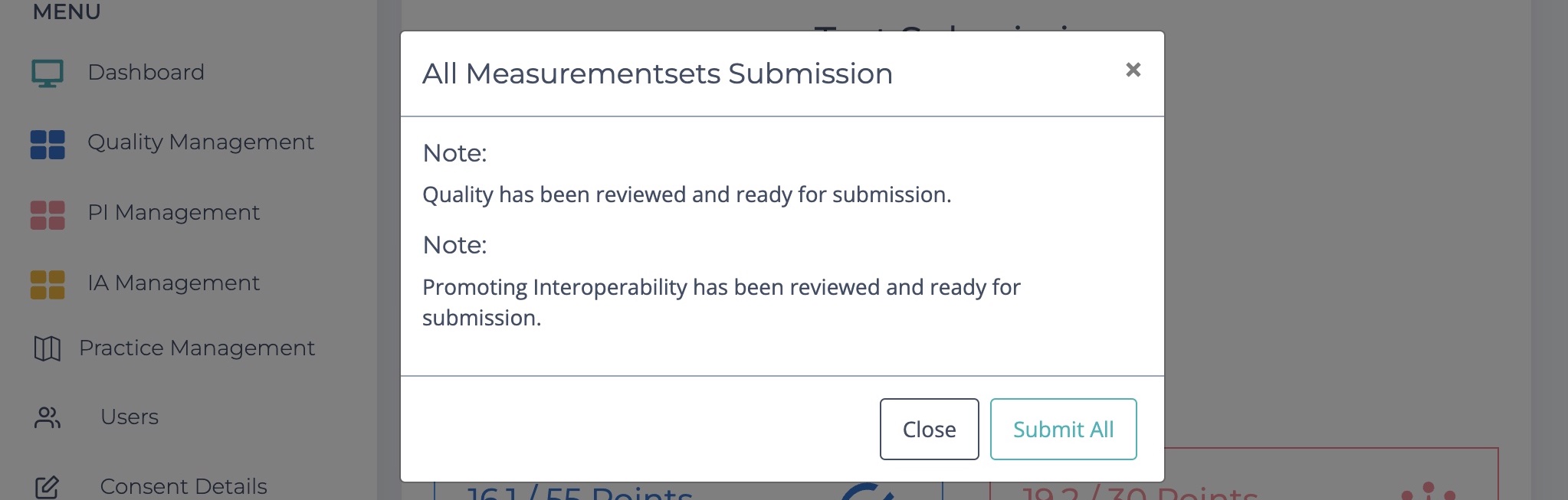
CQMsolution + Dynamic Qualified Registry
The Dynamic Qualified Registry seamlessly integrates CQMsolution with QPP, allowing users to submit CQMs with a single click.