Dynamic Qualified Registry
We are a CMS-approved MIPS/QPP Qualified Registry featuring expertise in CQM submission
Overview
As a CMS-approved Qualified Registry (QR) and your strategic partner for MIPS, we collect clinical data from MIPS-eligible clinicians (individuals, groups, and virtual groups) and submit this data to the Quality Payment Program (QPP). We support all three reporting options for QPP – Traditional MIPS, APP, and MVPs.
In addition to Clinical Quality Measures (CQMs), Dynamic Health IT (DHIT) can submit Promoting Interoperability (PI) metrics and practice Improvement Activities (IA). DHIT’s experts can also provide project management, technical guidance, and strategic support. Leverage our expertise for consulting on regulations to ensure ongoing compliance.
Features
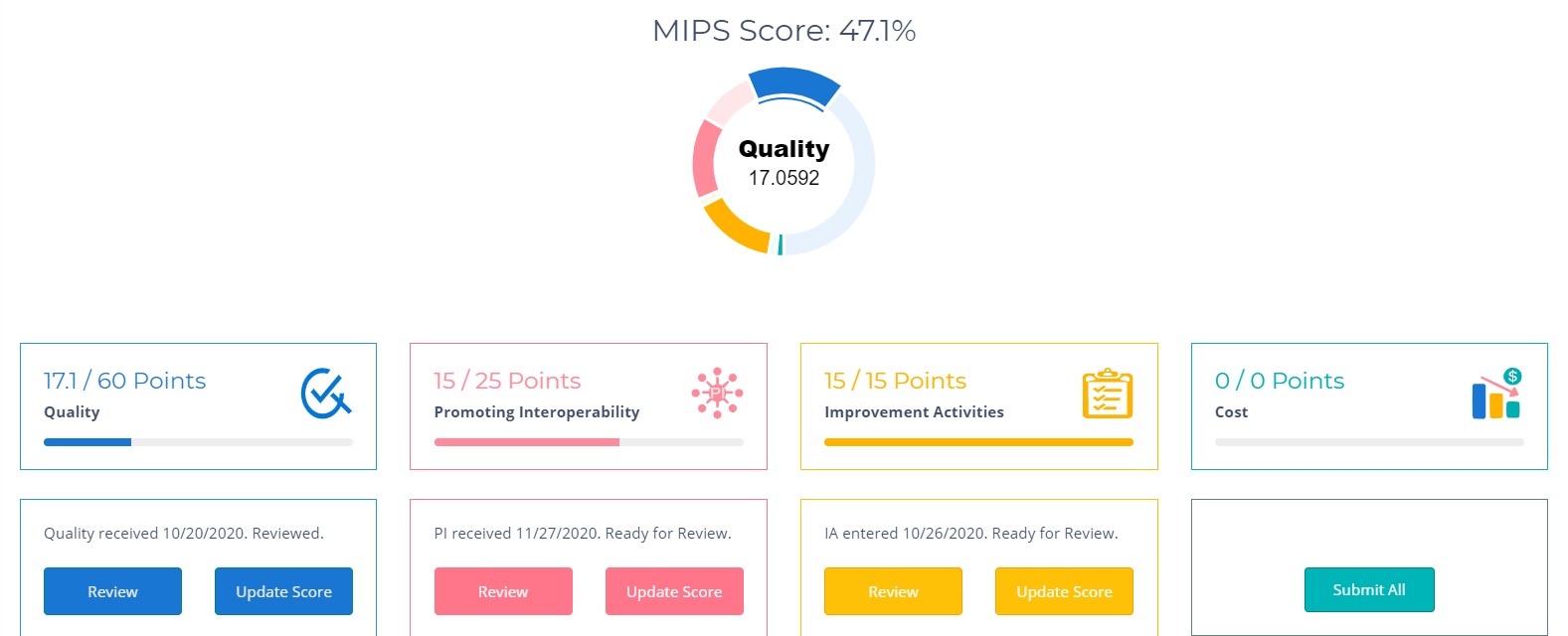
View Overall Performance
Our MIPS Registry dashboard displays overall MIPS score and each Measure Set performance
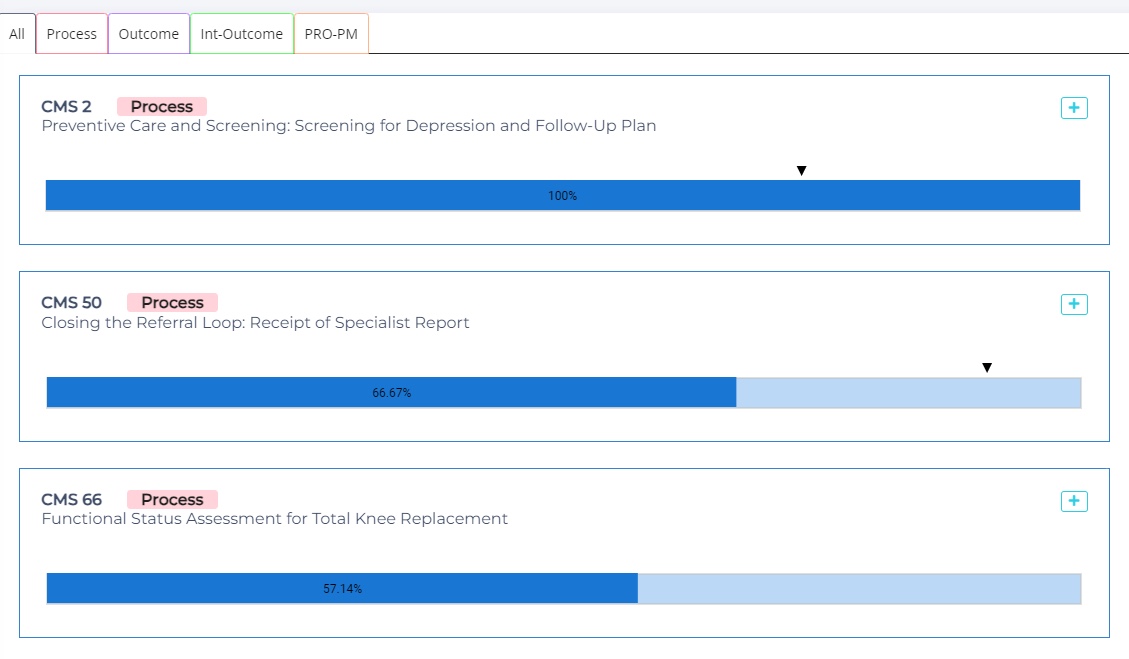
Analyze Each Quality Measure
The dashboard provides performance scores and benchmarks for each quality measure.
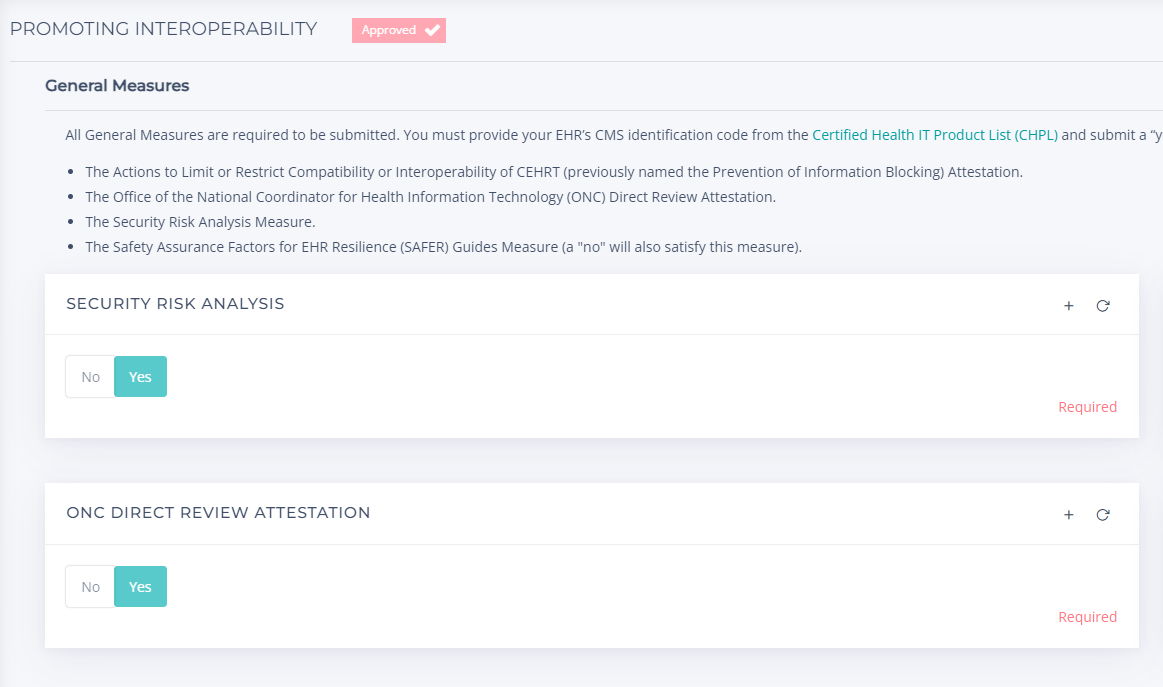
Promote Interoperability
See PI Numerator, Denominator, and Exclusions
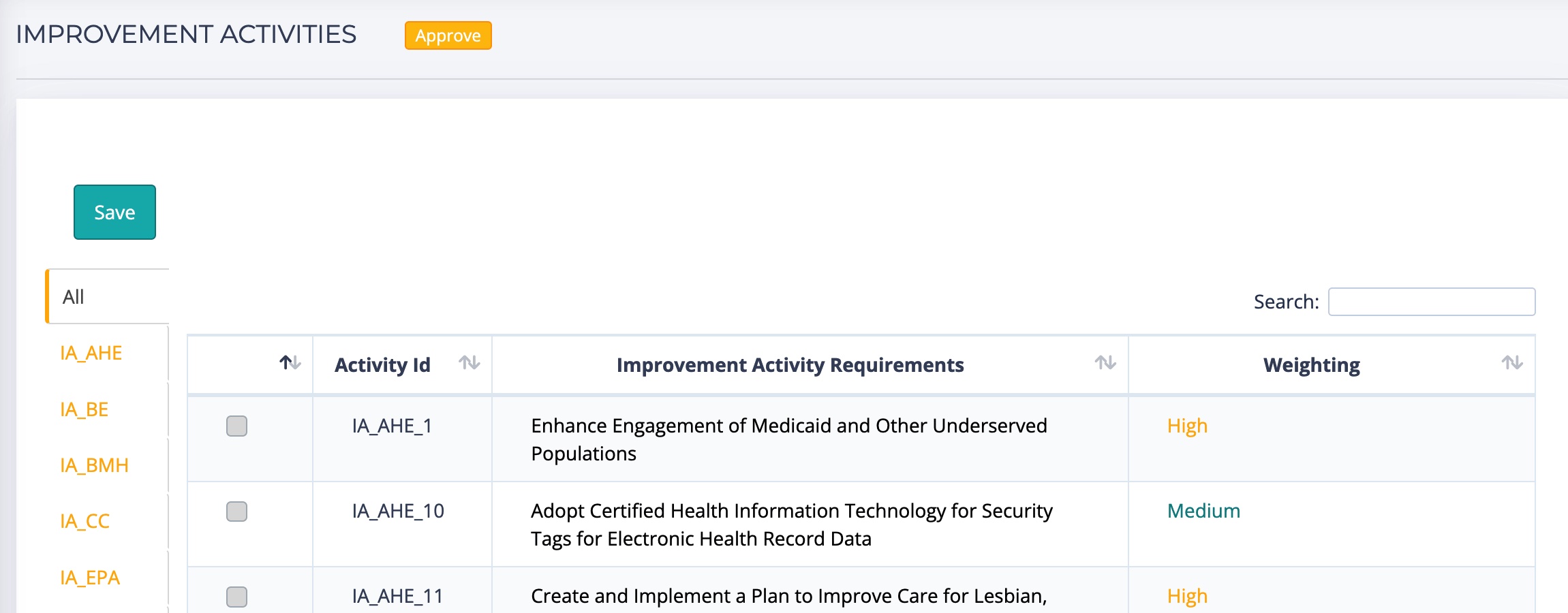
See Improvement Activities
View Improvement Activities and associated weights
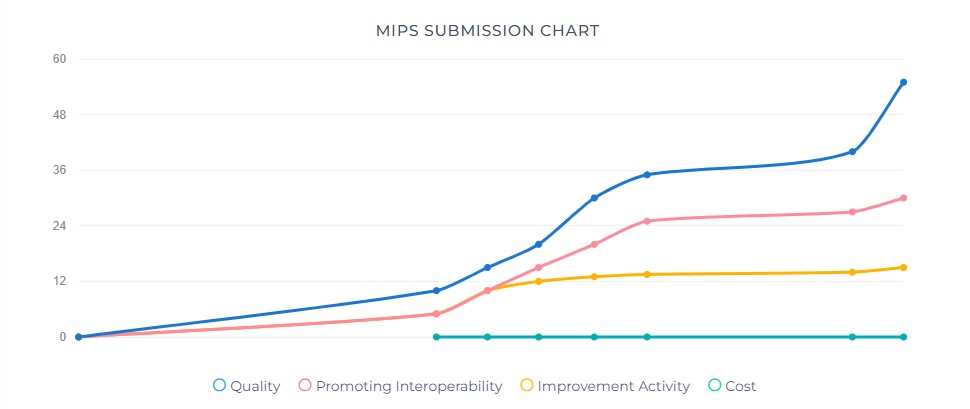
Track Scores over Time
MIPS Submission Chart gives snapshot of performance over time
How DHIT Can Help
A registry can simplify and improve the CQM submission process in a variety of ways since it:
- Reduces the burden on staff by providing expert technical and strategic support
- Includes project management to oversee data-gathering, testing and submission
- Optimizes your performance through quality measure selection and analysis of all available pathways to success
- Provides guidance on regulations to ensure ongoing compliance
- Streamlines and accelerates the MIPS submission process
We’re here for you!
Get in touch today about our Qualified Registry and other CQM calculation, analysis and submission services.
